Categories:

Four Myths, One Truth and the Way Forward for Addressing Maternity Deserts with Technology: Highlights from an Expert Maternal Health Panel
From maternal care deserts to OB-GYN shortages to unmet SDoH needs, more and more pregnant women are finding it difficult to get the care they need. Telehealth and other virtual tools have proven effective in extending the impact of clinical teams while creating higher levels of access and equity to women, regardless of their socioeconomic status or geographic location. The problem is that deploying the right technology in the right ways can be challenging.
During a recent webinar organized by The Health Innovation Company (Thinc), a multidisciplinary panel shared best practices and insights on how to use technology to close gaps in maternity care access. Panelists included the following:
This webinar tackled a range of questions and issues such as:
- How can payers and providers ensure they are using best practices and the best partners to support both the patient and local providers?
- How can they effectively monitor and mitigate risks sooner while keeping the care delivery ‘local’ and the entire care team on the same page?
- How can we create a sustainable economic model for care delivery in rural and underserved regions?
During this session, we dispelled several common myths about maternity deserts as we talked about insights and best practices. I thought it would be interesting to summarize this webinar by sharing four myths and one truth that we discussed as a panel.
To watch the full webinar, you can click here.
Myth 1: When we talk about maternity deserts, it’s really about gaps in access to facilities.
While rural hospitals continue to close across the country, this is only one layer of concern. The number of OB-GYNs also continues to dwindle, and the labor shortage disproportionately impacts rural communities. Additionally, sub-specialties such as maternal fetal medicine (MFM) practitioners are hard to come by in rural areas. All of this contributes to the expansive issue of maternity deserts. Consider the following facts:
- 2.2 million women of childbearing age live in a maternity desert.
- 2.5 million women of childbearing age live in a county without an obstetric provider (approximately half of all U.S. counties).
- Fewer than 7 percent of OB-GYN providers practice in rural areas, and with a national shortage of 22,000 OB-GYNs predicted in the coming years, this could decline further.
- The availability of MFMs closely tracks with the geographic distribution of OB-GYNS.
Compare the distribution of OB-GYNs and MFMs below in the maps shared by March of Dimes and Ouma Health.

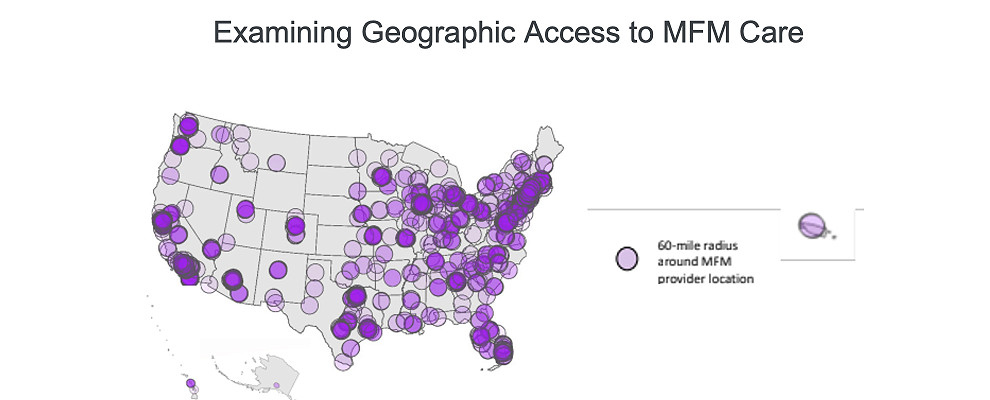
So in reality, it is not just hospitals and birthing centers, causing challenges, but also shortages of OB-GYNS and specialists such as MFMs who play an important role in assisting providers with high-risk pregnancies. At all levels, we are seeing a crisis in access to maternity care.
Myth 2: All rural areas are basically facing the same challenges and have the same needs.
Too often, we paint “rural America” with a broad brush. In reality, there are dramatically different circumstances and specific challenges to overcome based on the nuances of each geography.
For example, in some areas, you find instances of patients who are undocumented not willing to travel for appropriate care because they are afraid of being detained at border checkpoints. Meanwhile a woman living along the western border of Colorado has to journey all the way to Denver to see an MFM, instead of crossing the state line to Utah where there are high quality resources closer to her because of Medicaid reimbursement rules. Women on Indian reservations typically have to make a four hour drive, or more, to see a specialist. Even within the state of Texas, there are significantly different needs for communities in South Texas, compared to Central Texas or the Panhandle.
While it is important to develop solutions that can scale, we also have to build in flexibility so these solutions can address nuances at the local level. Cookie cutter solutions simply won’t cut it. There is no one-size-fits-all answer. Configurability of solutions is key.
Myth 3: Broadband access is the biggest barrier to using telehealth in rural counties.
Almost 1 in 5 U.S. counties (19.5%) have low telehealth access because of broadband issues. While access to broadband is very important, the reality is that broadband isn’t required to make progress with maternity deserts. Instead of fixating only on broadband, we should embrace a variety of other approaches that leverage more widely available technologies. As broadband access improves, more will be possible. In the meantime, our panel shared a laundry list of tactics that have shown results, including the following:
- Video conference solutions that work on a 3g signal
- Audio only consults to telephonically address patient issues
- Remote monitoring devices and in home visits
- Digital apps that are also available offline with education, resources and trackers
- Mobile maternal health units (pop up clinics, busses, etc.) that bring care to the community
- SMS helpline where women can text a central resource for assistance
- Empowering doulas to offer more support and bring information back to providers to coordinate care
Myth 4: Addressing maternity deserts is a costly proposition.
The reality here is both yes and no. Of course it will require a financial investment to address maternity deserts in a meaningful way. That cost can be offset by two factors: ROI, based on reduced costs, and value-based models that create a method for sustaining investment in new tools and approaches in a way that doesn’t add further expense to the system.
The data shows there is inherent value in closing care gaps by addressing maternity deserts. Mothers in rural areas have healthcare claims that are 15 percent higher (or more) compared to the general population. They also have higher rates of cesarean sections. Other studies have shown that in counties without MFM resources, women are twice as likely to have a premature birth. There is a very compelling ROI that supports investment in this area. Additionally, this ROI can be built in to a value-based model where all stakeholders are aligned and incented to deliver the best care to women. Value-based approaches in maternity care are growing in popularity across the country. This payment model plays a big role in supporting the flow of funds needed to address some of the most critical factors hampering maternal health outcomes in this country, including maternity deserts.
One last word on the financing of solutions. Despite record levels of funding in technology and innovation within the women’s health space, we have seen far too much emphasis on venture capital aimed at solutions built for employers or for higher income audiences, versus funding innovations squarely focused on those who are currently underserved. That trend has to change.
One Truth: Integration and collaboration are required for success.
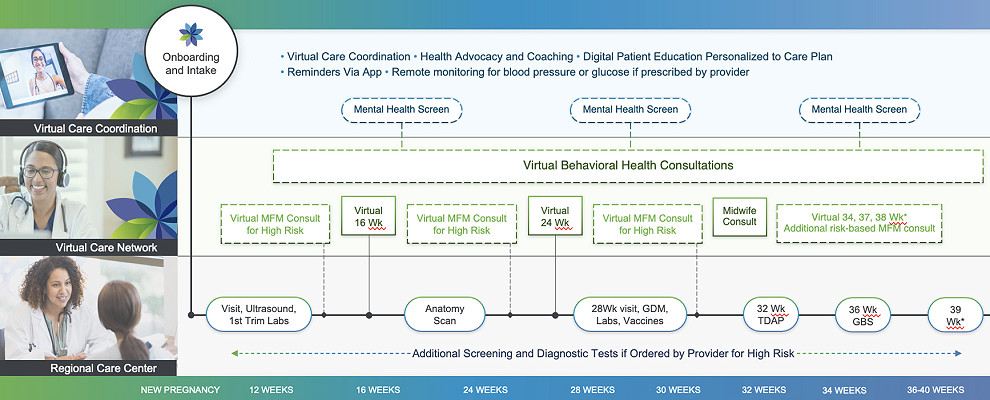
Our panel came up with a very powerful set of solutions for reaching patients in rural areas. But all of these standalone techniques and tools must be integrated in order to drive real change. That means integrated with each other, as well as with the provider who is ultimately responsible for the patient. We have to leverage a shared platform for specialized telehealth and virtual care collaboration that can easily plug in other resources where available, such as behavioral health support or pop up health clinics. We should be striving to create a hub and spoke model where the provider can serve as the medical home, while easily leveraging additional resources to support rural patients in a holistic way.
We also need deep collaboration among providers, payers, innovators and patients. This means aligning all parties and creating the ability to truly coordinate the best possible care. This includes maintaining a clear and complete view of patients – their needs, their activity and their data. The image below shows how a collaborative model with the OB-GYN as the hub for care could work.
Want to learn more about leveraging technology to combat maternity deserts and address SDoH needs? Click here to view the full webinar, or contact us today for a 1:1 consultation based on the nuances of the communities you support.
